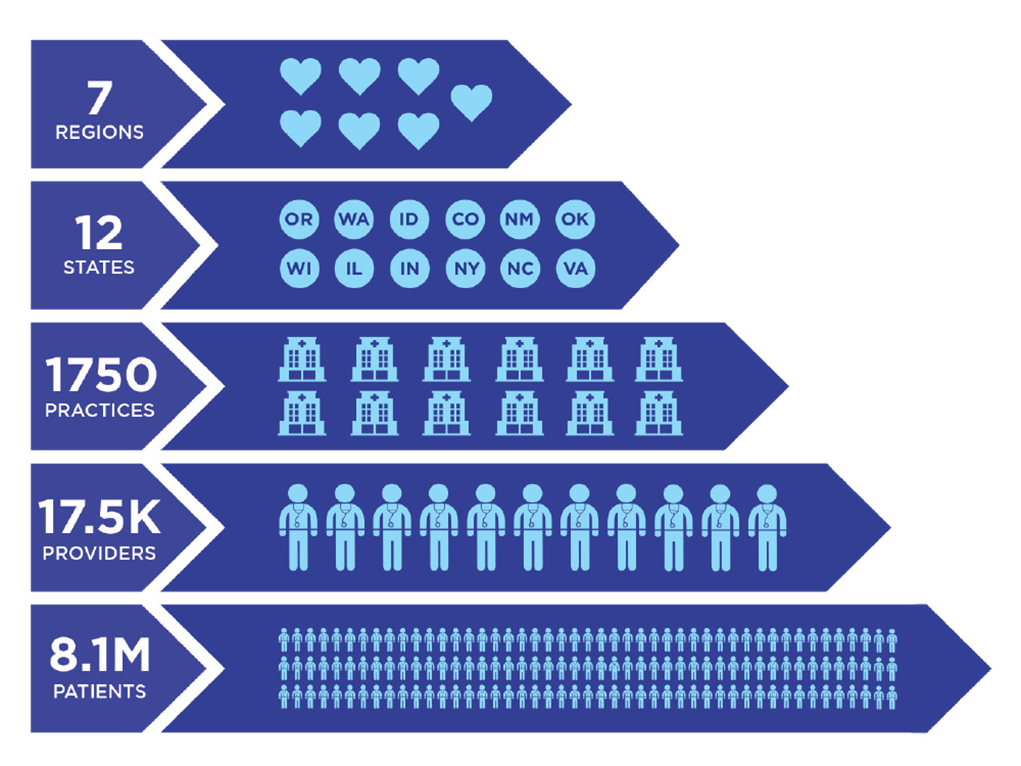
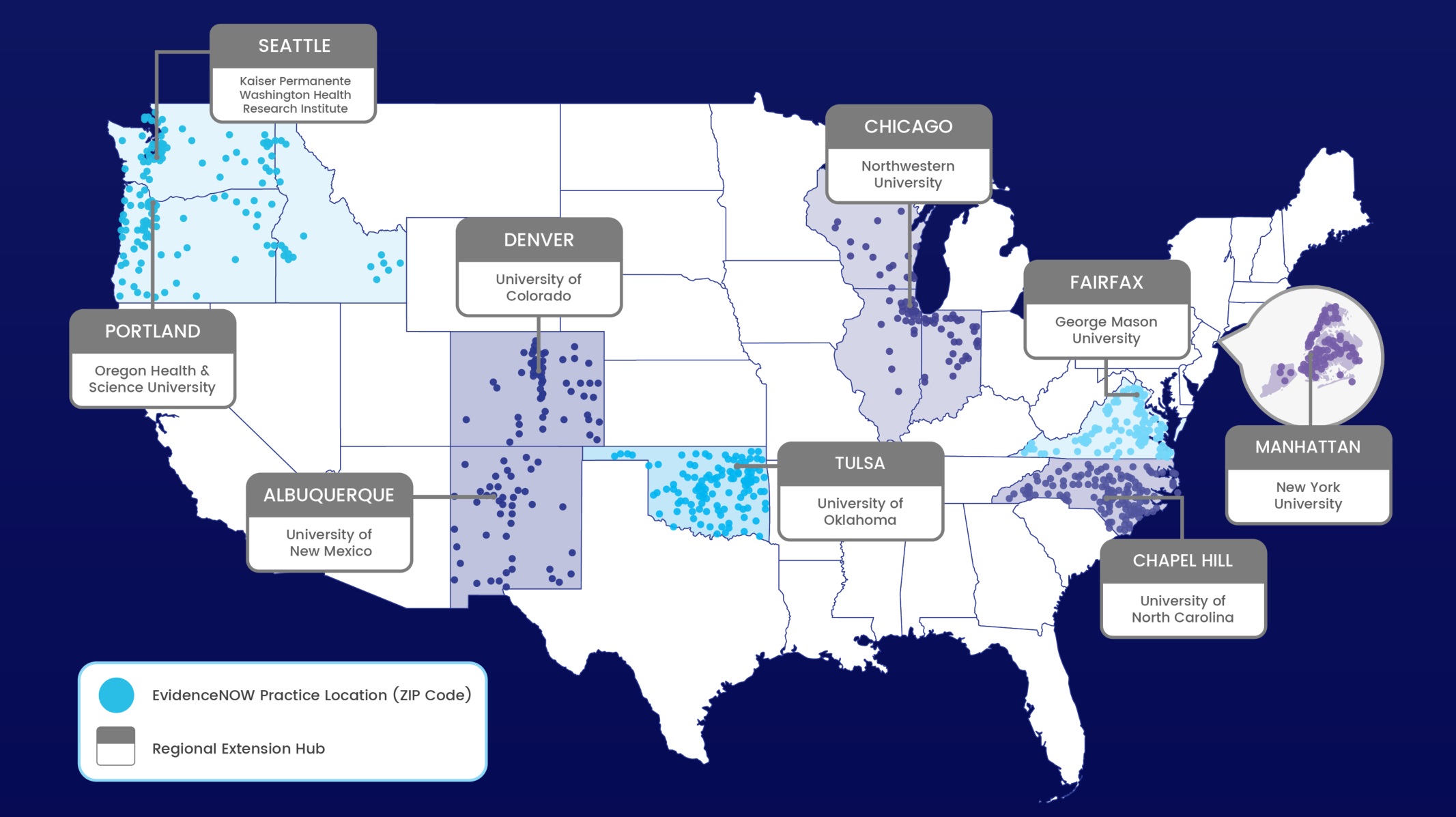
EvidenceNOW is focusing on helping primary care practices use the latest evidence to improve the heart health of Americans, and it is one of the largest initiatives funded by the Agency for Healthcare Research and Quality (AHRQ). EvidenceNOW is designed to transform cardiovascular healthcare delivery in the United States. By developing critical infrastructure, EvidenceNow will help thousands of primary healthcare providers translate innovative medical research findings into practice, improving the heart health of millions of Americans.
The EvidenceNOW Initiative includes a national evaluation, known as Evaluating System Change to Advance Learning and Take Evidence to Scale (ESCALATES). Led by Dr. Deborah Cohen, ESCALATES partnered with AHRQ and the seven regional cooperatives involved in the EvidenceNOW Initiative to conduct an evaluation that will inform large-scale dissemination and implementation (D&I) of evidence.
Primary Goals
- Engage cooperatives in the overall evaluation by harmonizing measures, working together to collect similar qualitative and quantitative data, identify lessons learned, and foster rapid-cycle learning
- Identify the practice, organization, and contextual factors among the combined 1,700 practices that are associated with meeting ABCS performance goals at baseline (prior to any intervention)
- Identify which intervention strategies are most effective in improving ABCS performance goals/targets over time in relation to practice, organization, and contextual factors and identify why some strategies are more effective
- Engage, rapidly disseminate, and evaluate the impact of disseminating actionable findings to key external stakeholders
ESCALATES used an innovative mixed methods approach to identify the most effective combinations of intervention strategies for various practice types, contexts, and organizational characteristics as well as understand why and how those combinations are effective.
Explore our recent findings to catch up on what ESCALATES has learned.